chapter
09
Gum Disease and the Overall Health Connection

Gums are just like skin, but on the inside. The gums cover and protect the teeth and jaw bone, and keep bacteria and other invaders from getting into the body. Also like skin, they can become damaged due to cuts, infections, disease and more. Let’s explore the key connection between your gums and your overall health.
Your gums are a part of the entire digestive system. The digestive system is a long tube that starts in the sinus cavities and nose and ends at the other end in the rectum.
If there is an infection anywhere along that system, the entire system is affected.
Many people suffer from digestive problems, and a big component of that is your gum health.
In fact, gum disease is the most common infection in the world, with estimates up to 80% of adults having some degree of infection in their gums.
Bottom line?
If you want to heal your gut and your body, you need to heal your gums too.
Jamie had always been a get-up-and-go kind of woman. Raising three girls of her own, running multiple businesses with her husband, and being a fabulous homemaker were all parts of her normal day.
Over the years she found she wasn’t able to do everything she once could, but she just thought it was part of getting older. Even though she was careful about what she was eating, she started gaining weight and couldn’t get it off. She was slowing down and started having aches and pains. And, the most worrisome part, she lost a few teeth that just got loose and came out.
Not knowing where to go, she visited a traditional dentist, who chastised her for not brushing her teeth well enough. Embarrassed and discouraged by this interaction, she avoided dentists and doctors for years until she was diagnosed with Type II diabetes and the pain in her body pushed her to do something.
She came to my office, where we found Stage Four gum disease along with advanced digestive and arthritic problems that related to the gum disease.
After cleaning the teeth, killing the microbes with a laser, and using ozone and nutrition that rebuilt her bone and gums, the gum disease was resolved. Treatment for her gut also helped her digestive symptoms, helped her reverse her diabetes, and allowed her to lose some weight.
She is now back on the road to feeling great again.
Gum Recession

Gum recession is a tell-tale sign of gum disease and something I check every time I complete an exam for a patient. Why?
It’s kind of like checking the pressure in your car tires. It’s a measuring stick for the health of the mouth, and if you find something a little off, you can quickly correct it before you get a flat tire!
There are two main reasons your gums may start to recede, and neither of them has to do with brushing too hard or getting older.
I bet at least 50% of the new patients I see with receding gums tell me a former dentist told them they were brushing their teeth too hard, and that is the reason for the gum problem.
The other 50% tell me they are just getting older and receding gums comes with the territory.
I’m going to have to disagree with both sides there!
Let’s talk about the real problems: Gum Disease and An Unbalanced Bite.
The two basic categories of gum disease are Gingivitis and Periodontitis.
Gingivitis – the official name for the gums is “gingiva”. And “it is” always means inflammation. So gingivitis means inflammation of the gums.
• This is the early stage of Gum Disease where the gums bleed easily and are swollen, but the disease has not progressed to the jawbone.
Periodontitis – Remember the ligament that connects your tooth to the bone? It’s called the periodontal ligament. This disease is inflammation of the periodontal ligament and the bone beneath. Periodontitis is inflammation of the bone and the gums.
• This is Stage 2-4 gum disease when the disease has progressed into the bone and there has been early to advanced bone loss, threatening the tooth and your overall health.
What Causes Gingivitis and Periodontitis?
Bacteria: The bacteria in your mouth like to congregate together. They live in the sticky substance on your teeth and tongue called plaque. The longer they stay in one place, the stickier these colonies get and more bacteria can join them.
Just as in any large city, the more people/bacteria that crowd together, the more garbage they create.
It’s the garbage (toxins) that inflame the gums.

Pay attention to where the plaque sticks. You’ll see it’s right around the gum line. If the plaque stays there for longer than a few days, the toxins start to damage the fragile gum tissue.
Your body, always on guard, sends its warriors there to battle this attack. That’s what inflammation is in a practical sense – your body’s reaction to a foreign invader. This particular form of inflammation is called gingivitis (see above).
Nutrition: There is another component to gum disease that has very little to do with bacteria. Early in the 19th century, sailors were stricken with scurvy as they sailed across the ocean with a very limited diet. One of the most prominent symptoms of scurvy is bleeding gums and loose teeth.
What was missing in these sailor’s diets? Vitamin C. If a Vitamin C deficiency could create a disease condition in the gums and bone, it’s obvious that nutrition plays a part in gum and bone health.
Other Causes
While bacteria and nutrition are the primary cause of gum disease, there are other factors that can contribute. These include:
- Hormonal changes, such as those occurring during pregnancy, puberty, menopause, and monthly menstruation, make the blood supply in the gum tissues more inflamed and the gums are more prone to bleeding and soreness.
- Illnesses may affect the condition of your gums. This includes cancer or autoimmune diseases that interfere with the immune system. Diabetes affects the body’s ability to use blood sugar, so patients with this disease are at higher risk of developing infections, including periodontal disease and cavities.
- Medications can affect oral health because some can decrease the flow of saliva, which has a protective effect on teeth and gums. Some drugs, such as the medication for epilepsy called Dilantin and some heart medications can lead to overgrowth of gum tissue.
- Bad habits such as smoking make it harder for gum tissue to repair itself.
- A family history of dental disease can be a contributing factor in the development of gingivitis.
How Gum Disease Arrives And Gets Progressively Worse

The startling fact is that more than 50% of the adult population in the US has some level of periodontal disease.
That means that one out of every two people has this infection. If left untreated, it can lead to inflammation and disease throughout the body.
Although most adults have some level of gum disease, very few people know it’s there.
Gingivitis is usually not painful. The gums turn red, they bleed when you brush, but they often don’t hurt.
The early warning system of pain is missing for this disease, which makes it more dangerous.
As gum disease progresses, eventually a pathway opens for the bacterial toxins to get to the bone beneath, which causes the bone to get infected and to start to recede as well.
The gums are lost, the bone is lost, and eventually, the tooth gets loose and can come out.
What a sorry tale!
And most of it happens with no pain to warn you beforehand.
I’ve often called periodontal disease the silent and deadly killer of teeth.
Some warning signs are bleeding gums when you brush, a bad taste in your mouth, loose teeth, and bad breath.
If you have any of these, run, don’t walk to the dentist! You don’t have any time to lose!
Key Signs Of Gum Disease:
- Bleeding Gums
- Sore Gums
- Bad Breath
- Loose Teeth
- Receding Gums
- Sensitive Teeth
Overall Health Effects of Periodontal Disease
Periodontal Disease is not something to wait on, because decades of scientific research have connected periodontal (gum) disease with other disease-including diabetes, high blood pressure, heart attacks, stroke, kidney and lung disease, cancer, infertility, erectile dysfunction, preterm birth, and other pregnancy complications.
People with periodontal disease have a 2x higher risk of dying from heart disease and a 3x higher risk of dying from a stroke. –Mayo Clinic
There is a significant connection between periodontal disease and Alzheimer’s disease. –Swiss research

There is a 64% increased risk of pancreatic cancer in those with periodontal disease –Harvard and Dana Farber Cancer Institute
Breast cancer is linked to periodontal disease –American Cancer Association
Diagnosis and Treatment of Gum Disease
Gum Exam
The health of your gums and bone should be measured at every cleaning, or what we call your “wellness visit”.
A special measuring tool is placed in this pocket to measure the depth of it. If it is deeper than 3 millimeters, that is a sign that the disease has ALREADY happened.
Bone has already been destroyed and the disease has progressed and has caused or is causing damage NOW. You should not wait to begin treatment as each day leads to further effects in the mouth and in the body.
Below are the treatment options for gum disease.
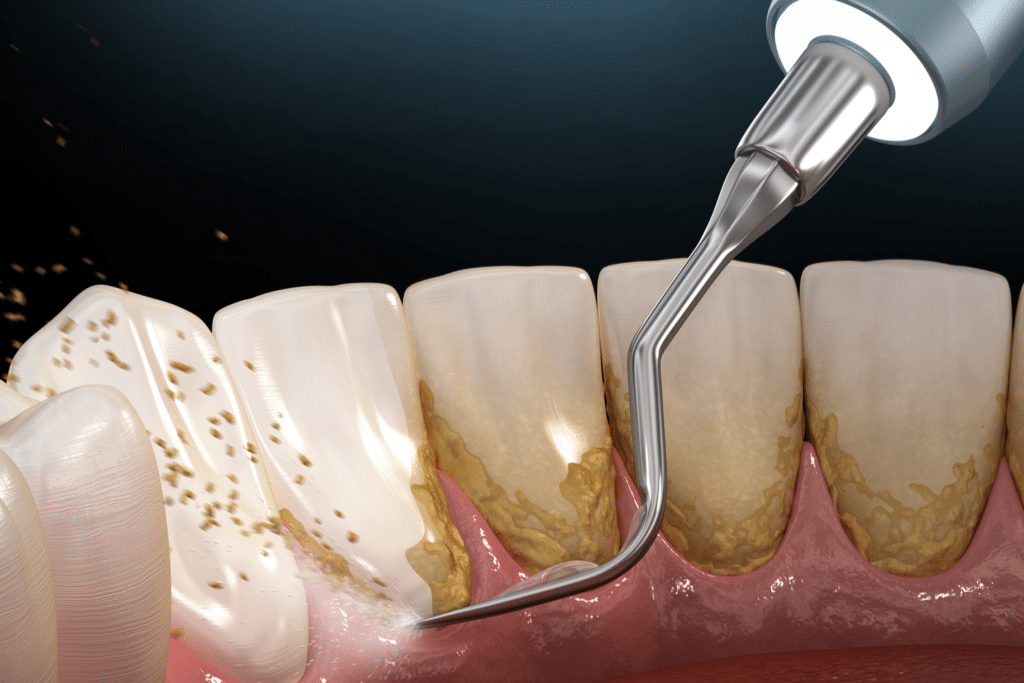
Mechanical cleaning:
The bacteria in your mouth creates a sticky layer on your teeth that, if not removed, calcifies and forms tartar that can’t be removed on your own. This tartar harbors other, more dangerous bacteria, and has to be removed if your gums and bone are to return to health.
The official name for this treatment is Scaling and Root Planing and is what is traditionally prescribed if you are diagnosed with gum disease. This cleaning can be done with traditional hand instruments, or with specialized ultrasonic instruments. Both can be utilized to remove all of the hard deposits on your teeth so your gums can heal.
Laser Cleaning and Disinfection:
Laser light energy is used to kill microbes over a large area of the infected root, gum tissue, and bone. This laser light is tuned into the harmful bacteria in the infected tissue, and up to 99.9% of the disease-producing bacteria are killed.
In addition to killing the bacteria and infection, the laser also stimulates stem cells in the tissues to form new connective tissues, collagen, and bone. Your body can then heal and rebuild these lost tissues.
Ozone Cleaning and Disinfecting:
Ozone is one of the most powerful natural oxidizing agents. It kills bacteria, disinfects, stops bleeding, and stimulates wound healing.
Used in a gas or liquid form, it has been shown to reduce bone loss and infection in 80% of periodontal disease areas, often significantly.
Being a gas, ozone is able to infiltrate the tissues, the smallest fissures, wounds, and the gum pockets, painlessly and without side effects.

Gum Irrigation:
Once the pockets around the teeth are clean, they can be treated with liquid medications to help the tissues heal and regenerate.
This procedure is called pocket irrigation and we use my remineralizing mouthwash infused with silver for this process.
I do not recommend using harsh antimicrobials such as Chlorhexidine, because of possible tissue damage.
Nutrition and Supplementation for Gum Disease Treatment
Vitamins and minerals, particularly the fat-soluble vitamins A, D3, E, K2, are essential to gum and bone health.
Read Chapter 3 of this guide to learn more about how to get these vitamins!
Though gum disease is always an infection caused by bacteria, poor nutrition often first sets the stage for that infection to occur.
Gum Disease Prevention
How do you prevent it? Do everything we talked about in the “Clean The Outside” section of Chapter Two.
If you take those few minutes each day, you can prevent most gum disease.
Add to that a healthy dose of Vitamin C and the other fat-soluble vitamins from the foods listed in Chapter Three, and your gums are nearly disease-proof.
You can also use my Remineralizing Mouthrinse daily for extra gum disease prevention!
Gums and How they Relate to the Bite and the Jaw Joint
This is the most misunderstood reason for receding gums.
If you have gum recession in an area that doesn’t have an infection, look at the tooth that hits against it when you bite. Does it have a recession too?
If so, these teeth are hitting too hard and causing the recession.
How does this happen?
If teeth hit together too hard or at an angle when chewing, the teeth rock. The gums start to pull away from the teeth as they are rocked, and part of the root that was below the gum becomes exposed.
The more the rocking happens, the more the gum pulls away and exposes the root.

This is, essentially, gum recession.
The tooth can become loose from this hitting and rocking, and can even be lost.
Why the recession is happening and how to fix it:
If the tooth is hitting too hard or at the wrong angle when biting, it needs to be “balanced”. This can be done very simply if only one or a few teeth are involved, by minimally reshaping the teeth to fit together better.
This can all be done here at Total Care Dental and Wellness, so come visit us and stay safe from gum disease!
Schedule Your New Patient Exam With Total Care Dental & Wellness
With a comprehensive exam, you’ll receive:
- A low dose cone beam 3d Dental Xray (CBCT)
- Tooth Xrays
- Dental photographs
- A comprehensive gum exam with an intraoral scan
- A comprehensive oral exam by a Total Care Doctor
- Jaw joint exam
- Oxygen, Sleep, and Airway Evaluation
You will leave the appointment with a report of findings and treatment recommendations from your doctor and care coordinator. Finances, scheduling, and other instructions will also be provided.